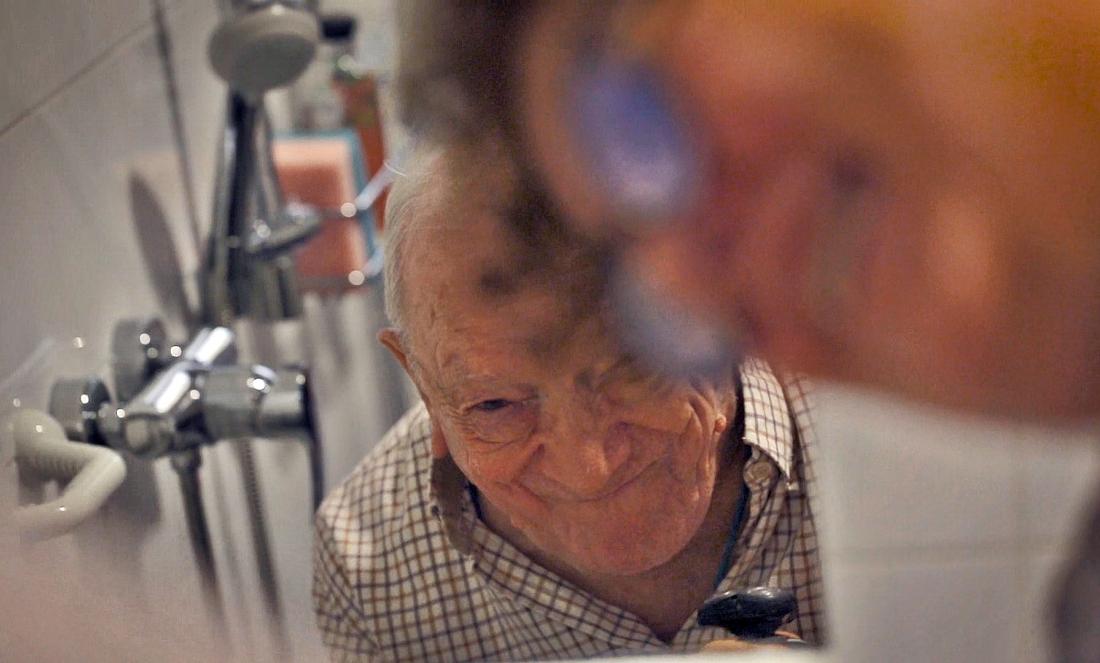
Bathroom and people with dementia. Hygiene and comfort versus the struggle of giants
Bathing in people with dementia is one of the most uncomfortable causes of care. The expression of this discomfort is reflected in different forms of agitation that lead to considerable overload for the caregiver. In this text we will try to explain the reasons for this discomfort, offering a series of guidelines that can help to ease the tension that accompanies this type of situation.
Confusion and fear, origin of rejection
In the residential environment, bathing can be a routine, depersonalised task, sometimes harmful to both the resident and the carer. While most people with dementia tend to tolerate this process well, the suggestion to take a shower is not always equally welcome.
As you know, in a few years we have gone from carrying out hygiene in bed to a bathroom with adapted areas, which involves taking the person with dementia to that space, undressing them, soaping them...
The person with dementia may not understand the need for such activity and may be afraid and confused. It is in these cases that, when insisted upon, the feared behavioural disorders (in the form of shouting, physical agitation, psychomotor restlessness...) arise.
For the caregiver, often aware of what awaits him/her, bath time becomes an added stress factor that stirs up his/her fear, anxiety, frustration and conditions the coexistence of both.
Knowing that hygiene is related to uses and customs, intimacy and individual preferences, an approach that could help in these cases would be to know the person's previous hygiene habits, as well as the presence of language alterations (comprehension capacity), sphincter incontinence, inappropriate sexual behaviour, visual or auditory sensory deprivation, etc.
Thus, in the case of Luis, who has been a baker all his life and has the habit of getting up and washing up very early, he may not be comfortable with a schedule that does not suit his usual lifestyle. Similarly, Maria, who has always been very modest, will accept the situation better if another woman helps her in the bathroom.
To our knowledge, pharmacological intervention for the control of this type of disruptive behaviour has been relatively ineffective, to which should be added the high risk of adverse drug reactions. Because of this, it seems logical that the approach should be primarily behavioural, educating and training carers in something that perfectly illustrates the title of Barrick et al.
In addition, we must take into account other aspects such as the number of people, the gender of the carer, the technical aids needed, characteristics of the bath, noise and ambient temperature.
In short, the important thing is not the performance of the activity itself, but to generate the minimum possible discomfort to the person, understanding that bathing is a basic care with hygienic (cleanliness, smell), psychological and emotional effects (feeling of well-being).
General guidelines that can help at bath time:
- It simplifies the task as much as possible. It can help to establish a sequential order.
- Plan everything in advance, knowing and taking into account the preferences of each person.
- It guarantees the privacy of the person at all times. Nobody likes to have an audience while bathing. Explain the procedure with simple words and a collaborative attitude.
- Install safety elements and suitable chairs, without leaving the resident alone at any time to avoid risks to his/her safety (falls, fractures, accidents with bathroom utensils).
- Maintain an adequate temperature of the water and the environment. It is highly recommended to have a gradual contact with the water temperature. In selected cases, the use of hygiene mittens (they have non-irritating soap, emollient cream and water, and do not require subsequent drying), minimises behavioural disorders*.
- Establish cleaning rituals, starting with the extremities, the front and back of the trunk, the genitals and the head. It favours the person's autonomy at all times. Whatever he or she can do alone, he or she should do it at his or her own pace. Haste is not a good ally. If there is resistance to performing the hygiene, look for another more favourable moment.
- Take care of both verbal and non-verbal communication. It is advisable to use simple, short sentences, familiar terms,... All this accompanied by gestures and words that transmit tranquillity, relaxation, interest in the person.
- Make sure that the atmosphere is comfortable and calm. Avoid noises that may disturb the person. In some cases it can be useful to play relaxing music, taking advantage of the moment for a positive and pleasant interaction in the established intimacy.
- In case of uneasiness, it reassures the person. We can distract them by focusing attention on pleasant aspects that are pleasing to them. In the event of an overloaded caregiver, he or she will rotate the assistants.
- Establishes a flexible schedule. Seeks the best possible moment by establishing prudent limits regarding the periodicity of care.



Add new comment