
Keys to a good night's rest for people with dementia living in gerontological centres
Sleep disorders and dementia
People spend a third of their lives sleeping, with sleep having a physical and cognitive repair function. As the years go by, the time dedicated to this activity gradually decreases. Night-time awakenings increase, sleep becomes more superficial, sedentariness increases and there is a tendency to rest in the form of naps.
In people with dementia, sleep is disturbed from the early stages, due to the pathological changes of this syndrome and especially due to the concomitant pathologies, medicines and environmental changes.
The frequent presence in the elderly of pain, cramps/tingling, fatigue, coughing, reflux, nocturia, or the taking of medication such as bronchodilators, diuretics, corticoids, hypotension, different psycho-pharmaceuticals, largely condition the ability to maintain a restful sleep. It is estimated that up to 42% of adults present insomnia, 70% may have obstructive sleep apnoea (38% in severe degree), being relevant these frequencies in people with neurological diseases (dementia, Parkinson, stroke) or psychiatric diseases. The consequences are relevant in terms of decreased quality of life, increased disability and risk of falls, increasing mortality, and constitutes a relevant cause of institutionalisation given the overload it entails for the caregiver.
What to pay attention to and what to do
It is important to know each person's sleeping habits (the time they usually go to bed and get up, the time they spend until they wake up, the time they spend awake...), as well as the physical activity they do throughout the day, the exposure to the sun, the type of social relationships they have and their participation in activities.
In gerontological centres, it is key to define sleep disorders well (problems of initiation or maintenance, behavioural alterations, abnormal movements, respiratory alterations, advanced or irregular circadian rhythm). We will pay attention to all those aspects that alter rest and induce the appearance of this type of disorders in people who live in these homes: noise, temperature, changes imposed on sleep in relation to care (taking of constants, absorbent changes, administration of medication, diabetic prescriptions, postural changes...), as well as the consequences that derive from these alterations and for whom (resident or carers). In this way we can make an initial approach between the person's sleep disorder and the flexibility or capacity of the centre to adapt to their needs.
Among the possible measures to be adopted, we can design an intervention plan based on basic hygiene and stimulus control measures; provide behavioural training sessions; and, finally, favour a structured pharmacological intervention, with pre-established objectives and duration (clinical trials usually last between 6 and 8 weeks of treatment, not indefinitely), assessing at all times the risk-benefit balance of the different interventions.
The number of night-time caregivers is significantly lower than during the day, so that the sleep changes due to ageing and the different comorbidities promote an excess of pharmacological interventions, with a high risk of adverse reactions (falls, confusional syndrome, dizziness...).
There are experiences of multifactorial interventions in residents with dementia that are effective*. Below is a list of them.
Decalogue of good practices to favour a correct rest of people who live in residences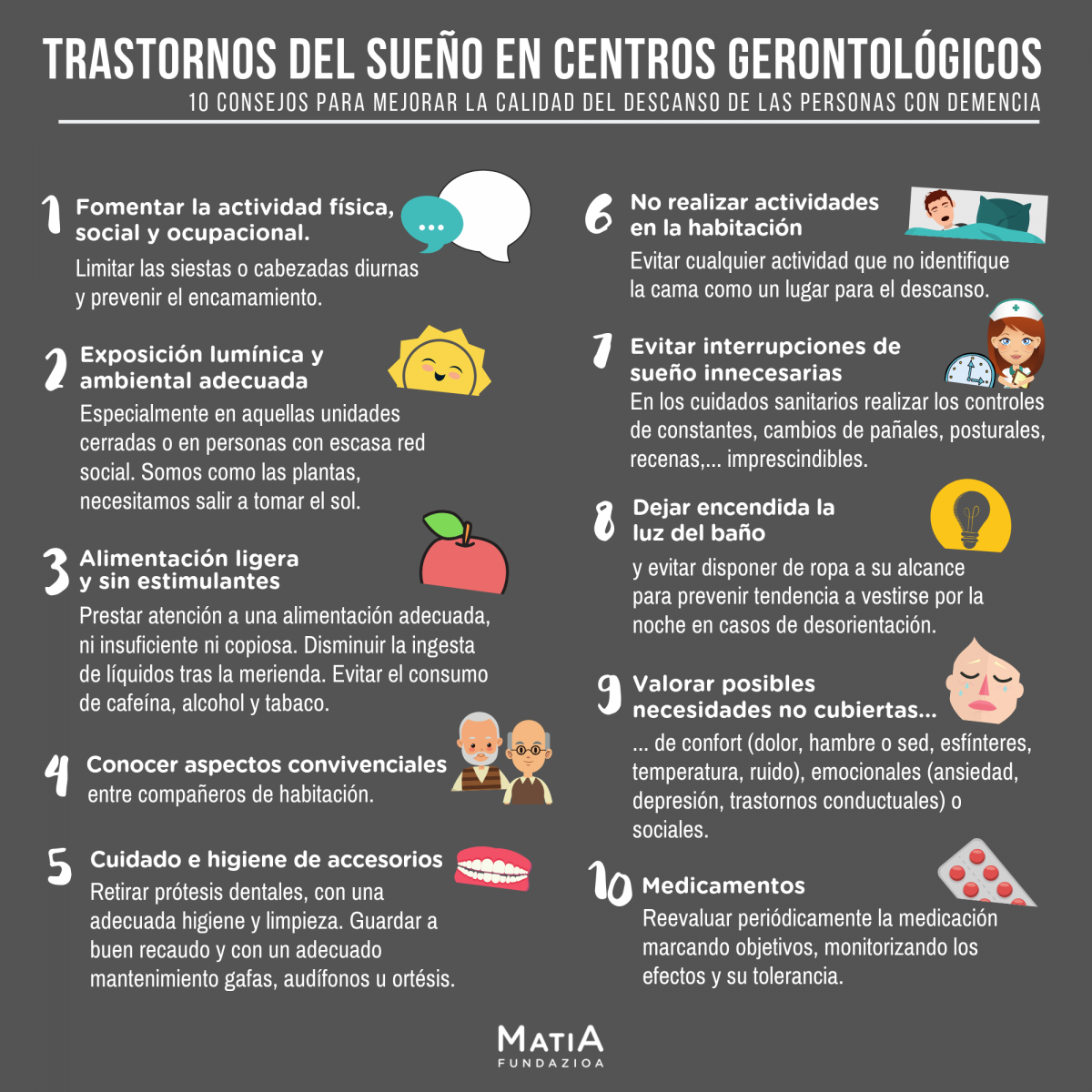
- Encourage physical, social and occupational activity. Limit daytime naps or napping and prevent bedding.
- Adequate light and environmental exposure, especially in closed units or in people with little social network, guaranteeing outdoors.
- Light food without stimulants. Pay attention to an adequate diet, neither insufficient nor copious. Reduce the intake of liquids after a meal. Do not take stimulant substances such as coffee, tobacco, alcohol or medicines that interfere with sleep.
- To learn about living together with your roommates.
- Care and hygiene of accessories. Maintain the care of the mouth, removing dental prostheses, with adequate hygiene and cleanliness. Keep spectacles, hearing aids or orthotics in good condition and with adequate maintenance.
- Do not carry out activities in the room, such as watching television, being with pets, identifying the bed as a place to sleep.
- Avoid interruptions of sleep to administer medication or health care (control of constants, nappy changes, postures, prescriptions) that are not essential.
- Leave the bathroom light on. Avoid having clothes within your reach to prevent a tendency to dress at night in cases of disorientation.
- Assess possible unmet needs. Pay attention to aspects related to comfort: pain, hunger or thirst, sphincters, temperature, noise, comfort, lighting..., as well as emotional aspects: anxiety, depression, behavioural or social disorders.
- Periodically re-evaluate medications for the control of chronic pathologies, the use of hypnotic drugs according to the type of insomnia, setting objectives, monitoring the effects and their tolerance.


Add new comment