From Matia we feel the need to share a series of guidelines for the emotional care of carers and relatives of people who require support and who are living the current situation of confinement both in a centre and in their homes.
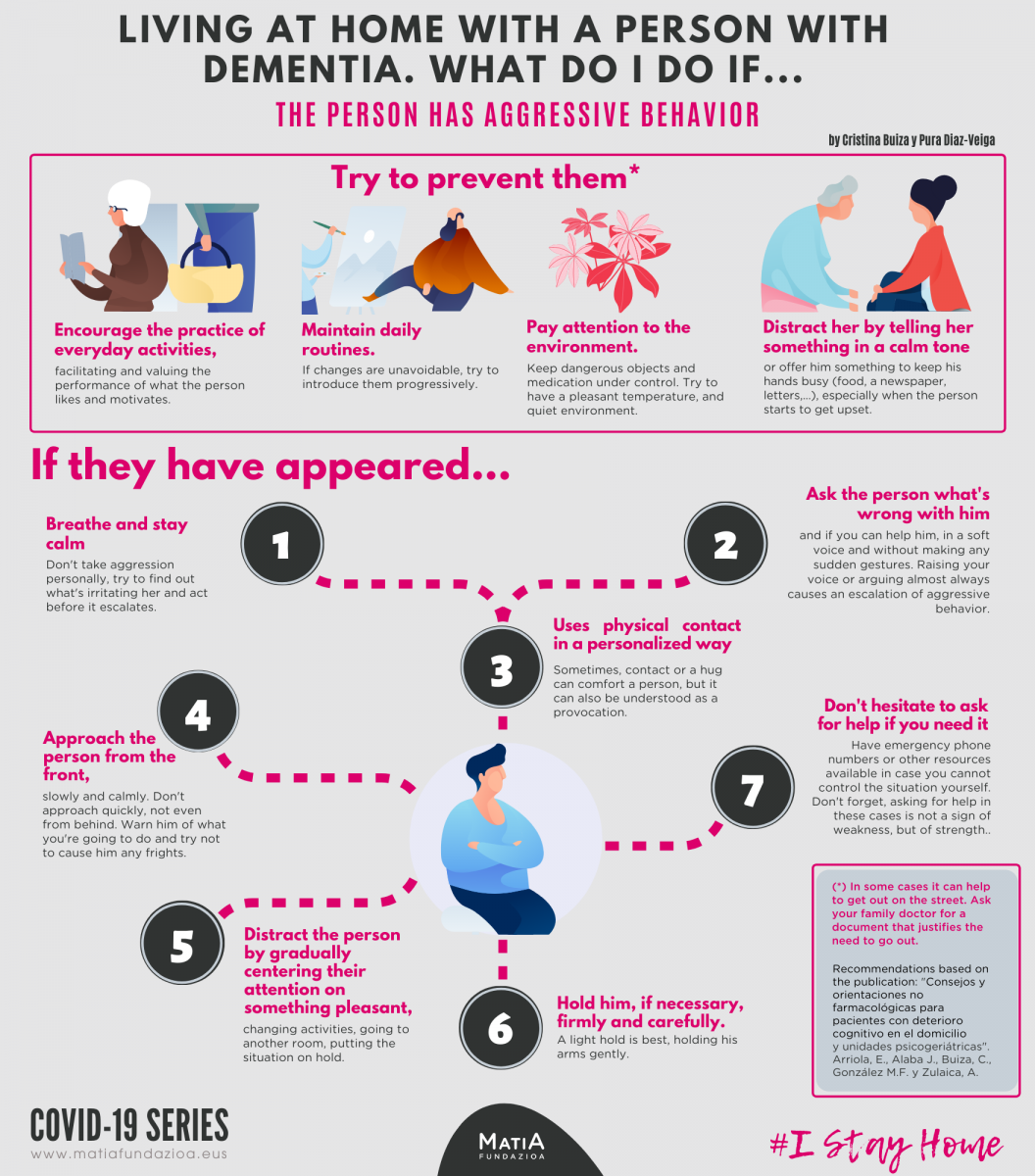
LIVING AT HOME WITH A PERSON WITH DEMENTIA. WHAT DO I DO IF...THE PERSON HAS AGGRESSIVE BEHAVIOR
- Breathe and stay calm Don't take aggression personally, try to find out what's irritating her and act before it escalates.
- Ask the person what's wrong with him and if you can help him, in a soft voice and without making any sudden gestures. Raising your voice or arguing almost always causes an escalation of aggressive behavior
- Uses physical contact in a personalized way Sometimes, contact or a hug can comfort a person, but it can also be understood as a provocation.
- Approach the person from the front, slowly and calmly. Don't approach quickly, not even from behind. Warn him of what you're going to do and try not to cause him any frights.
- Distract the person by gradually centering their attention on something pleasant, changing activities, going to another room, putting the situation on hold.
- Hold him, if necessary, firmly and carefully. A light hold is best, holding his arms gently.
- Don't hesitate to ask for help if you need it. Have emergency phone numbers or other resources available in case you cannot control the situation yourself. Don't forget, asking for help in these cases is not a sign of weakness, but of strength
(*) In some cases it can help to get out on the street. Ask your family doctor for a document that justifies the need to go out. Recommendations based on the following readings: "Consejos y orientaciones no farmacológicas para pacientes con deterioro cognitivo en el domicilio y unidades psicogeriátricas". Arriola, E., Alaba J., Buiza, C., González M.F. y Zulaica, A.
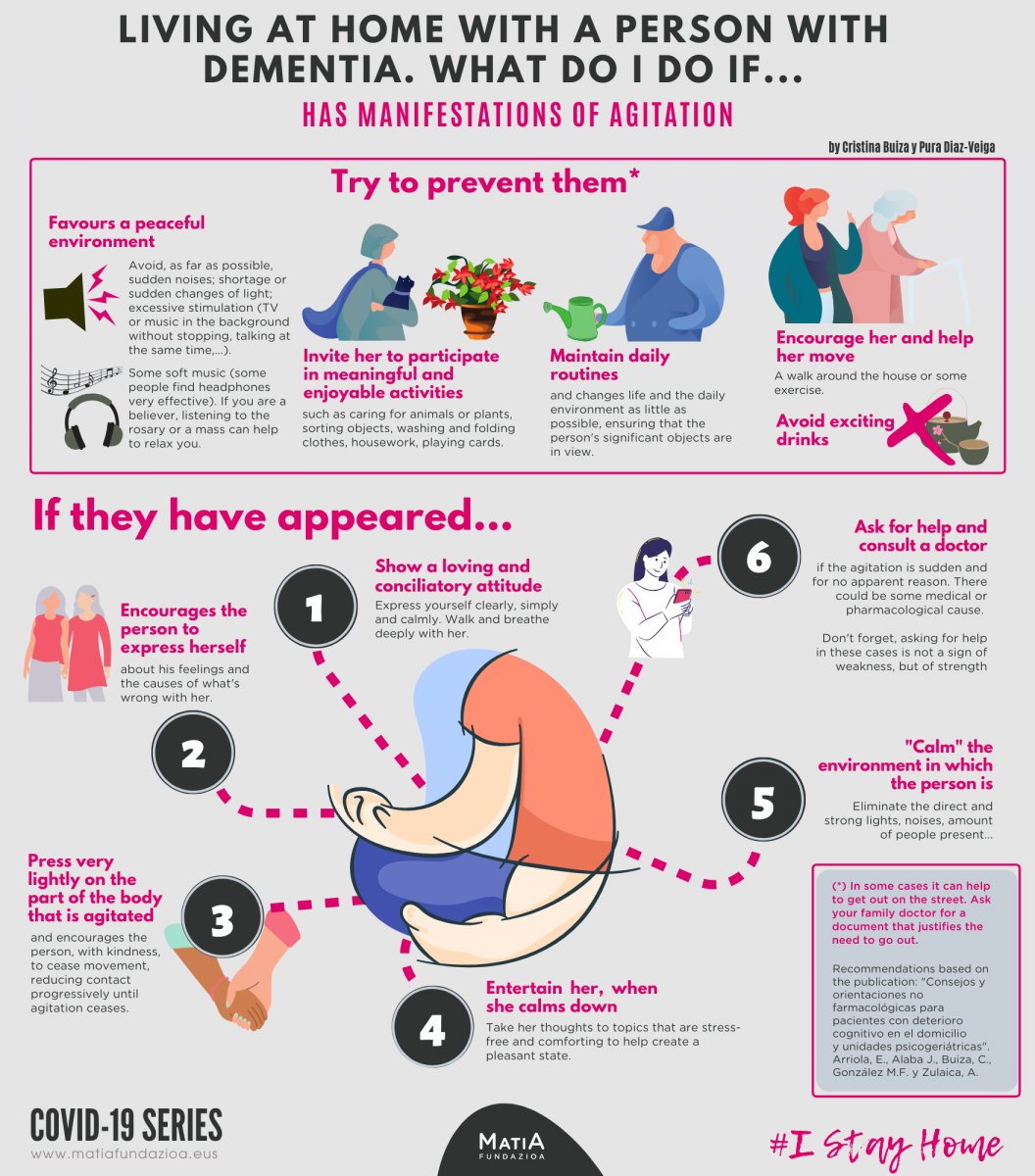
LIVING AT HOME WITH A PERSON WITH DEMENTIA. WHAT DO I DO IF...THE PERSON HAS MANIFESTATIONS OF AGITATION
Try to prevent them (*)
- Favours a peaceful environment. Avoid, as far as possible, sudden noises; shortage or sudden changes of light; excessive stimulation (TV or music in the background without stopping, talking at the same time,...). Some soft music (some people find headphones very effective). If you are a believer, listening to the rosary or a mass can help to relax you.
- Invite her to participate in meaningful and enjoyable activities such as caring for animals or plants, sorting objects, washing and folding clothes, housework, playing cards.
- Maintain daily routines and changes life and the daily environment as little as possible, ensuring that the person's significant objects are in view.
- Encourage her and help her move. A walk around the house or some exercise.
- Avoid exciting drinks.
If they have appeared...
- Show a loving and conciliatory attitude. Express yourself clearly, simply and calmly. Walk and breathe deeply with her.
- Encourages the person to express herself about his feelings and the causes of what's wrong with her.
- Press very lightly on the part of the body that is agitated and encourages the person, with kindness, to cease movement, reducing contact progressively until agitation ceases.
- Entertain her, when she calms down. Take her thoughts to topics that are stress-free and comforting to help create a pleasant state.
- "Calm" the environment in which the person is. Eliminate the direct and strong lights, noises, amount of people present...
- Ask for help and consult a doctor if the agitation is sudden and for no apparent reason. There could be some medical or pharmacological cause. Don't forget, asking for help in these cases is not a sign of weakness, but of strength.
(*) In some cases it can help to get out on the street. Ask your family doctor for a document that justifies the need to go out. Recommendations based on the following readings: "Consejos y orientaciones no farmacológicas para pacientes con deterioro cognitivo en el domicilio y unidades psicogeriátricas". Arriola, E., Alaba J., Buiza, C., González M.F. y Zulaica, A.
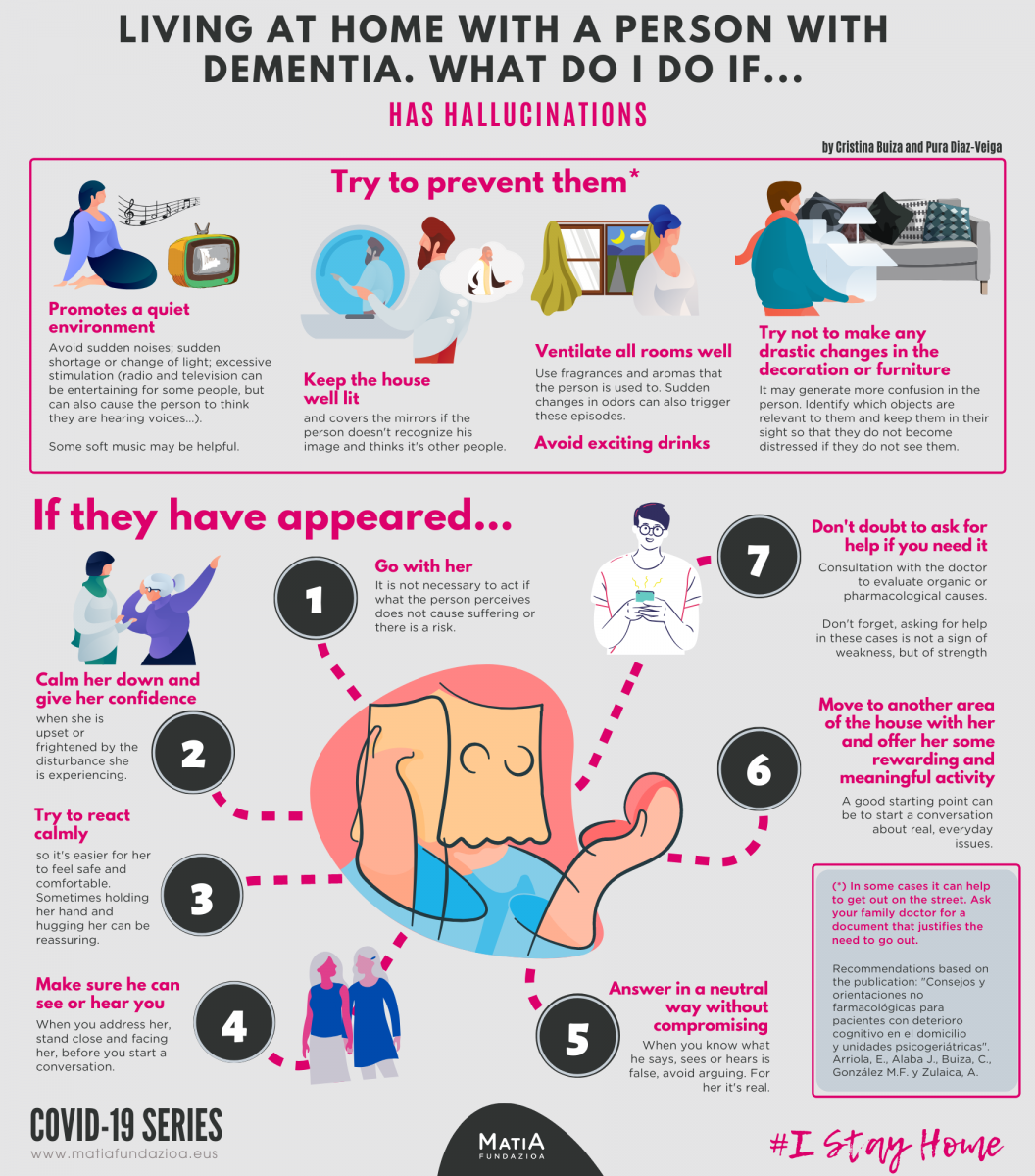
LIVING AT HOME WITH A PERSON WITH DEMENTIA. WHAT DO I DO IF...THE PERSON HAS HALLUCINATIONS
Try to prevent them (*)
- Promotes a quiet environment. Avoid sudden noises; sudden shortage or change of light; excessive stimulation (radio and television can be entertaining for some people, but can also cause the person to think they are hearing voices...). Some soft music may be helpful.
- Keep the house well lit and covers the mirrors if the person doesn't recognize his image and thinks it's other people.
- Ventilate all rooms well. Use fragrances and aromas that the person is used to. Sudden changes in odors can also trigger these episodes.
- Avoid exciting drinks
- Try not to make any drastic changes in the decoration or furniture. It may generate more confusion in the person. Identify which objects are relevant to them and keep them in their sight so that they do not become distressed if they do not see them.
If they have appeared...
- Go with her. It is not necessary to act if what the person perceives does not cause suffering or there is a risk.
- Calm her down and give her confidence when she is upset or frightened by the disturbance she is experiencing.
- Try to react calmly so it's easier for her to feel safe and comfortable. Sometimes holding her hand and hugging her can be reassuring.
- Make sure he can see or hear you. When you address her, stand close and facing her, before you start a conversation.
- Answer in a neutral way without compromising. When you know what he says, sees or hears is false, avoid arguing. For her it's real.
- Move to another area of the house with her and offer her some rewarding and meaningful activity. A good starting point can be to start a conversation about real, everyday issues.
- Don't doubt to ask for help if you need it. Consultation with the doctor to evaluate organic or pharmacological causes. Don't forget, asking for help in these cases is not a sign of weakness, but of strength.
(*) In some cases it can help to get out on the street. Ask your family doctor for a document that justifies the need to go out. Recommendations based on the following readings: "Consejos y orientaciones no farmacológicas para pacientes con deterioro cognitivo en el domicilio y unidades psicogeriátricas". Arriola, E., Alaba J., Buiza, C., González M.F. y Zulaica, A.
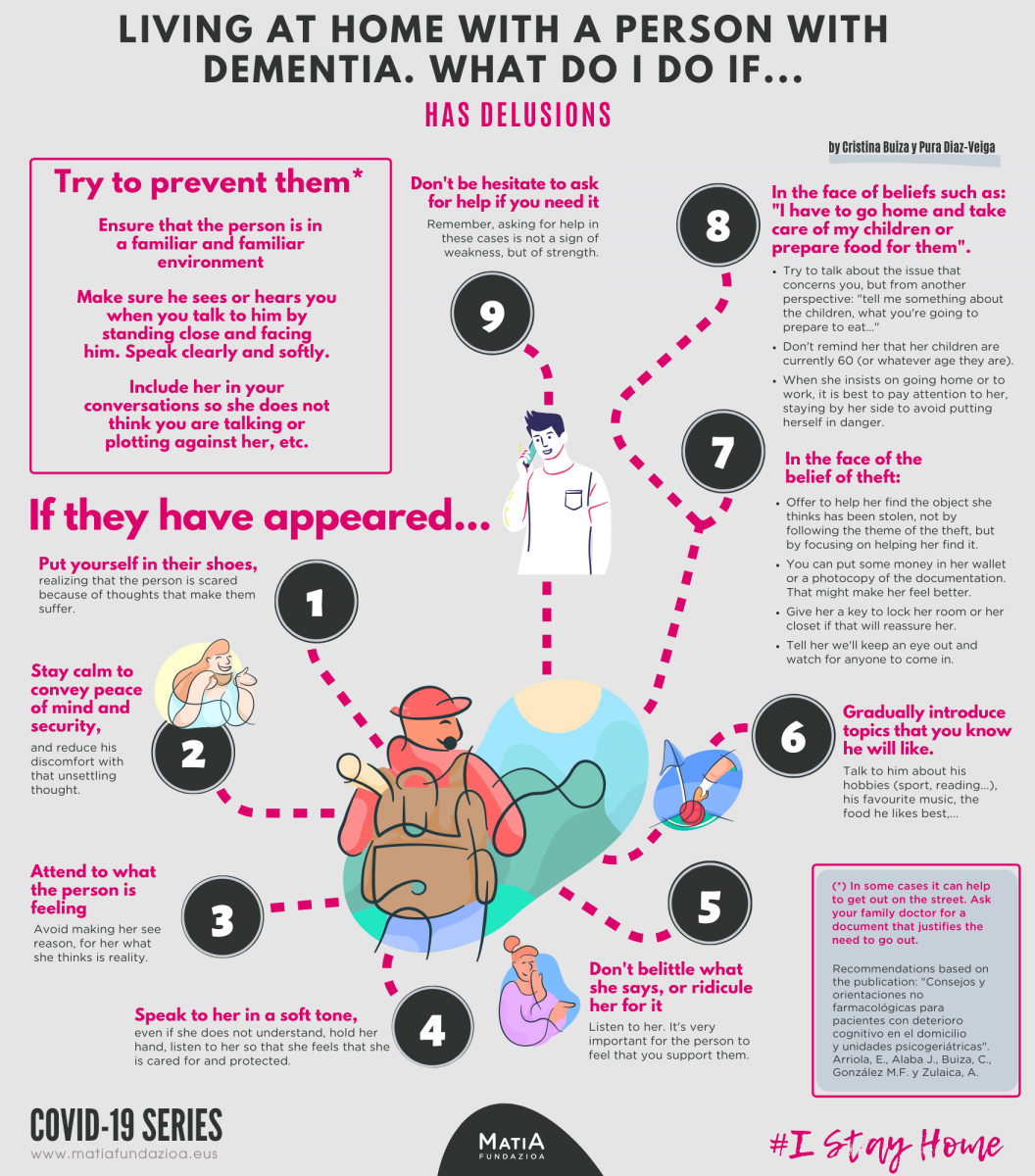
LIVING AT HOME WITH A PERSON WITH DEMENTIA. WHAT DO I DO IF...THE PERSON HAS DELUSIONS
Try to prevent them (*)
- Ensure that the person is in a familiar and familiar environment.
- Make sure he sees or hears you when you talk to him by standing close and facing him. Speak clearly and softly.
- Include her in your conversations so she does not think you are talking or plotting against her, etc.
If they have appeared...
- Put yourself in their shoes, realizing that the person is scared because of thoughts that make them suffer
- Stay calm to convey peace of mind and security, and reduce his discomfort with that unsettling thought.
- Attend to what the person is feeling. Avoid making her see reason, for her what she thinks is reality.
- Speak to her a soft tone, even if she does not understand, hold her hand, listen to her so that she feels that she is cared for and protected.
- Don't belittle what she says, or ridicule her for it. Listen to her. It's very important for the person to feel that you support them.
- Gradually introduce topics that you know he will like. Talk to him about his hobbies (sport, reading...), his favourite music, the food he likes best,...
- In the face of the belief of theft:
- Offer to help her find the object she thinks has been stolen, not by following the theme of the theft, but by focusing on helping her find it.
- You can put some money in her wallet or a photocopy of the documentation. That might make her feel better.
- Give her a key to lock her room or her closet if that will reassure her.
- Tell her we'll keep an eye out and watch for anyone to come in.
- In the face of beliefs such as: "I have to go home and take care of my children or prepare food for them".
- Try to talk about the issue that concerns you, but from another perspective: "tell me something about the children, what you're going to prepare to eat..."
- Don't remind her that her children are currently 60 (or whatever age they are).
- When she insists on going home or to work, it is best to pay attention to her, staying by her side to avoid putting herself in danger.
- Don't be hesitate to ask for help if you need it. Remember, asking for help in these cases is not a sign of weakness, but of strength.
(*) In some cases it can help to get out on the street. Ask your family doctor for a document that justifies the need to go out. Recommendations based on the following readings: "Consejos y orientaciones no farmacológicas para pacientes con deterioro cognitivo en el domicilio y unidades psicogeriátricas". Arriola, E., Alaba J., Buiza, C., González M.F. y Zulaica, A.
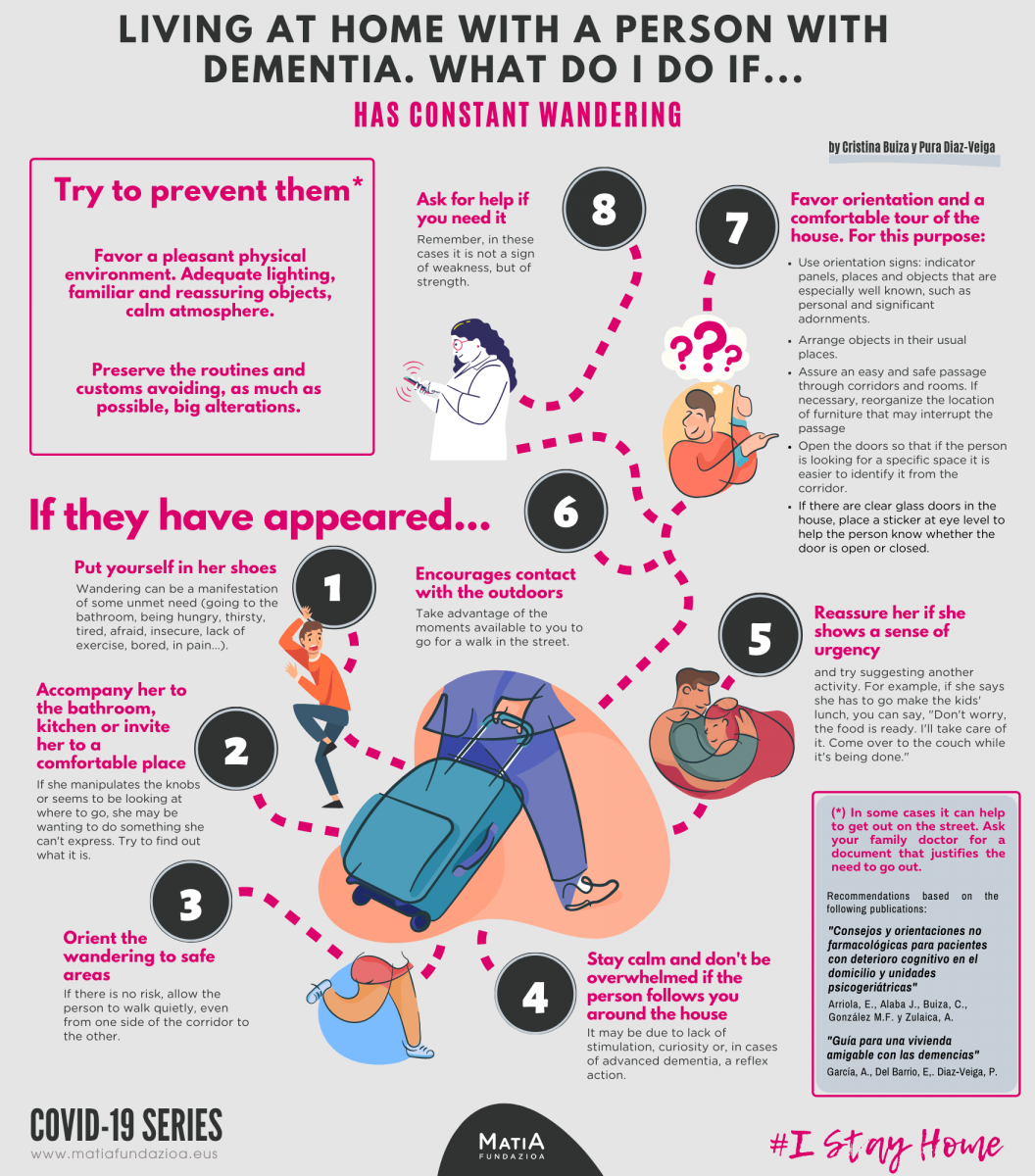
LIVING AT HOME WITH A PERSON WITH DEMENTIA. WHAT DO I DO IF...THE PERSON HAS CONSTANT WANDERING
Try to prevent them (*)
- Favor a pleasant physical environment. Adequate lighting, familiar and reassuring objects, calm atmosphere.
- Preserve the routines and customs avoiding, as much as possible, big alterations.
If they have appeared...
- Put yourself in her shoes. Wandering can be a manifestation of some unmet need (going to the bathroom, being hungry, thirsty, tired, afraid, insecure, lack of exercise, bored, in pain).
- Accompany her to the bathroom, kitchen or invite her to a comfortable place. If she manipulates the knobs or seems to be looking at where to go, she may be wanting to do something she can't express. Try to find out what it is.
- Orient the wandering to safe áreas. If there is no risk, allow the person to walk quietly, even from one side of the corridor to the other.
- Stay calm and don't be overwhelmed if the person follows you around the house. It may be due to lack of stimulation, curiosity or, in cases of advanced dementia, a reflex action.
- Reassure her if she shows a sense of urgency and try suggesting another activity. For example, if she says she has to go make the kids' lunch, you can say, "Don't worry, the food is ready. I'll take care of it. Come over to the couch while it's being done."
- Encourages contact with the outdoors. Take advantage of the moments available to you to go for a walk in the street.
- Favor orientation and a comfortable tour of the house. For this purpose:
- Use orientation signs: indicator panels, places and objects that are especially well known, such as personal and significant adornments.
- Arrange objects in their usual places.
- Assure an easy and safe passage through corridors and rooms. If necessary, reorganize the location of furniture that may interrupt the passage.
- Open the doors so that if the person is looking for a specific space it is easier to identify it from the corridor.
- If there are clear glass doors in the house, place a sticker at eye level to help the person know whether the door is open or closed.
- Ask for help if you need it. Remember, in these cases it is not a sign of weakness, but of strength.
(*) In some cases it can help to get out on the street. Ask your family doctor for a document that justifies the need to go out. Recommendations based on the following readings: "Consejos y orientaciones no farmacológicas para pacientes con deterioro cognitivo en el domicilio y unidades psicogeriátricas". Arriola, E., Alaba J., Buiza, C., González M.F. y Zulaica, A.
LIVING AT HOME WITH A PERSON WITH DEMENTIA. WHAT DO I DO IF...SHE SHOWS INAPPROPIATE SEXUAL MANIFESTATIONS
Try to prevent them (*)
- Favor a pleasant and quiet environment. Certain content offered by television can over-stimulate the person.
- Help to create, if that is what the person wishes, spaces and times for intimacy.
If they have appeared...
- Put yourself in her shoes. Try to understand and minimize these situations. Rule out causes like irritations, infections... That the person is undressing may respond to being hot, wanting to go to the bathroom or feeling some discomfort, for example.
- Keep calm. Reacting naturally promotes the person's peace of mind. Remember that this behavior is a manifestation of the disease.
- Offer conversation. Sometimes sexual behavior reflects a need for interaction with another person. Lead that need into a conversation or other shared activity.
- Redirect sexual expression into activities that help the person focus on something else. For example, get some physical exercise. Sometimes simple distractions, such as offering some water or juice, can also help.
- What do I do if the person...
- ... gets into my bed. Redirect him to his room. This behavior may stem from a search for non-sexual intimacy or simply from disorientation.
- … appears naked. Cover him up with a robe and take him somewhere private without giving him any importance. His behavior may be because he is hot or needs to go to the bathroom. Or he just needs activity and that's what's available to him at that time.
- … masturbates in public. Try to stay calm and lead her to a private place without giving her too much importance. Don't scold her, don't embarrass her.
- ... makes touches to other people. Explain directly to her that such behavior is not appropriate with that person or place. Firmly, but without getting into arguments or confrontations.
- ... flirts by making offensive comments and/or inappropriate gestures. This behavior may be linked to old social roles. Remind the person, in a kind and practical way, that this behaviour is not acceptable, giving them opportunities to re-experience their social role in other aspects.
- Ask for help as soon as you feel you need it. Remember, in these cases it is not a sign of weakness, but of strength.
(*) In some cases it can help to get out on the street. Ask your family doctor for a document that justifies the need to go out. Recommendations based on the following readings: "Consejos y orientaciones no farmacológicas para pacientes con deterioro cognitivo en el domicilio y unidades psicogeriátricas". Arriola, E., Alaba J., Buiza, C., González M.F. y Zulaica, A. / "Desinhibición sexual. Pautas de abordaje". Gracia, P.
.png)
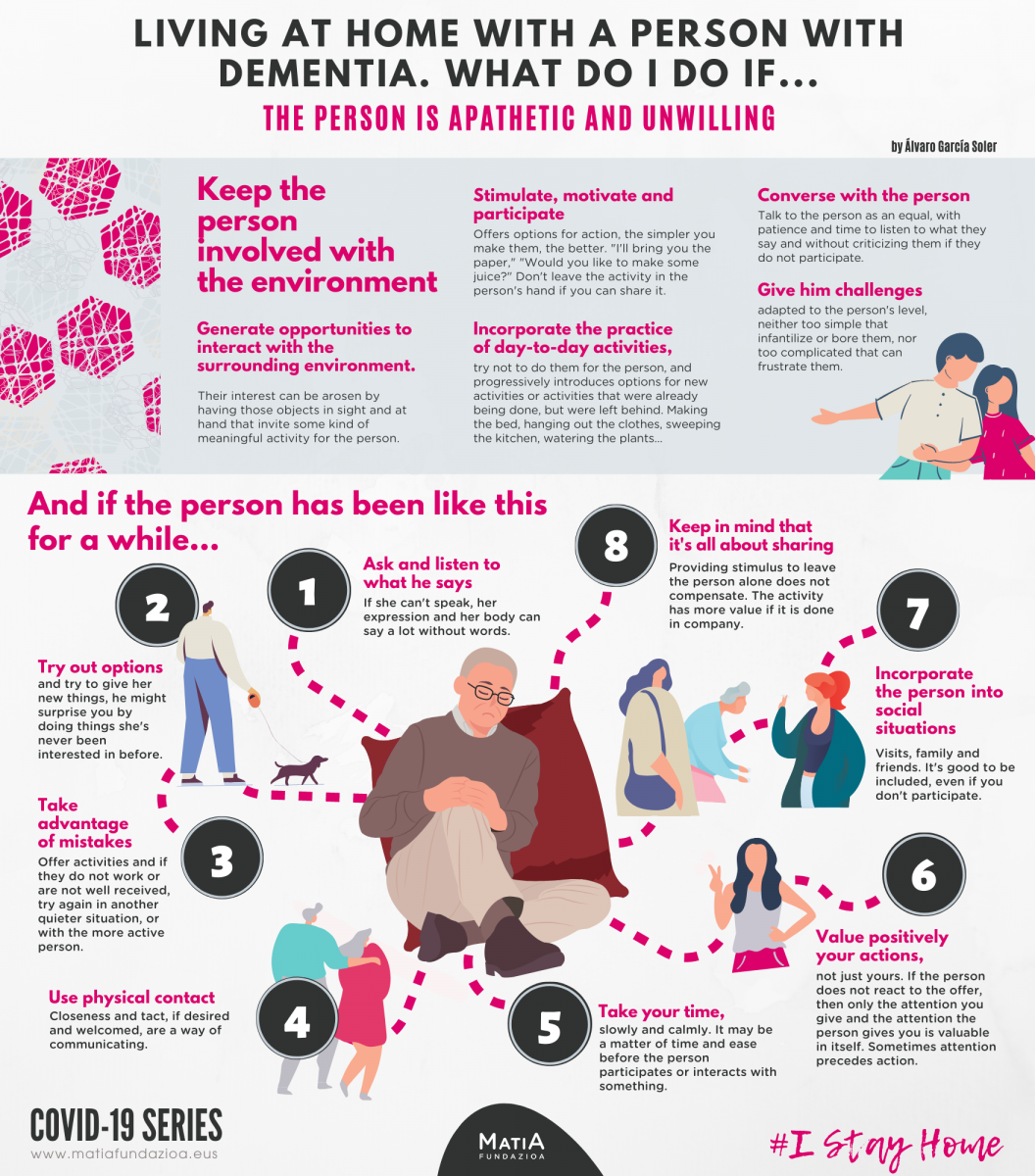
LIVING AT HOME WITH A PERSON WITH DEMENTIA. WHAT DO I DO IF...
The person is apathetic and unwilling
KEEP THE PERSON INVOLVED WITH THE ENVIRONMENT
- Generate opportunities to interact with the surrounding environment. Their interest can be arosen by having those objects in sight and at hand that invite some kind of meaningful activity for the person.
- Stimulate, motivate and participate. Offer options for action, the simpler you make them, the better. "I'll bring you the paper," "Would you like to make some juice?" Don't leave the activity in the person's hand if you can share it.
- Incorporate the practice of day-to-day activities, try not to do them for the person, and progressively introduces options for new activities or activities that were already being done, but were left behind. Making the bed, hanging out the clothes, sweeping the kitchen, watering the plants...
- Converse with the person. Talk to the person as an equal, with patience and time to listen to what they say and without criticizing them if they do not participate.
- Give him challenges adapted to the person's level, neither too simple that infantilize or bore them, nor too complicated that can frustrate them.
AND IF THE PERSON HAS BEEN LIKE THIS FOR A WHILE...
- Ask and listen to what he says. If she can't speak, her expression and her body can say a lot without words.
- Try out options and try to give her new things, he might surprise you by doing things she's never been interested in before.
- Take advantage of mistakes. Offer activities and if they do not work or are not well received, try again in another quieter situation, or with the more active person.
- Use physical contact. Closeness and tact, if desired and welcomed, are a way of communicating.
- Take your time, slowly and calmly. It may be a matter of time and ease before the person participates or interacts with something.
- Value positively your actions, not just yours. If the person does not react to the offer, then only the attention you give and the attention the person gives you is valuable in itself. Sometimes attention precedes action.
- Incorporate the person into social situations. Visits, family and friends. It's good to be included, even if you don't participate.
- Keep in mind that it's all about sharing. Providing stimulus to leave the person alone does not compensate. The activity has more value if it is done in company.
10 RECOMMENDATIONS IF YOUR OLDER RELATIVE IS IN ISOLATION AT HOME
- Maintain a daily contact routine. through a phone call, video conference or any other secure means for you and your family member.
- Try to maintain a positive and affectionate tone. Reassure him/her about your condition and the condition of the people he/she cares about.
- Encourage him/her to do his/her personal care routines. Hygiene, clothing, medication, some exercise,... If you know of any meaningful activities she does, invite her to continue them.
- Make sure she eats right and has her medications. Send her the food, if necessary prepared, and taking into account her preferences.
- Entertainment is important. Give her the magazines, the newspapers she likes. You can also bring her a movie or, if she likes music, a CD.
- Send her photos of family members, voice notes, via WhatshApp... If she does not have WhatsApp you can send her a family photo with a message of encouragement on the back. Send them along with food and medicine
- Remind him of his strength in dealing with past situations. Older people carry a large rucksack of experience with them and many have overcome difficult situations in the past.
- Encourage them to contact friends and neighbours. Many will be in similar situations and can share their experiences and concerns with each other.
- Listen to them and answer their questions. Give her the information she requests that will help her.
- If possible, divide this contact with the older relative among several acquaintances. Its good for the person and also for the rest of the family.

10 TIPS FOR THOSE WHO CANNOT STAY AT HOME BECAUSE THEY ARE CARING
- Focus on the day-to-day. Life goes on for you and the person you care for.
- Never more than now does the team matter. Consult, share and agree.
- Be aware of your abilities to solve situations. Trust yourself.
- An exceptional situation requires exceptional ideas, in good care too.
- Ask for help if you need it. We are part of a team that works best when it supports each other.
- Take, whenever you can, small breaths. Rest is an essential part of good care.
- Don't forget. Every day is a triumph. Adding to negative thoughts won't make normality return any sooner.
- Eat well, rest as much as you can and enjoy your people. The latter by taking the necessary precautions.
- We take care of ourselves, we take care of lives. Mutual and reciprocal care helps us to develop our work: to accompany lives, lives in progress.
- Receive the gratitude of the people you care for, their families and that of citizens committed to good care.

10 RECOMMENDATIONS IF YOU TAKE CARE OF A PERSON WITH DEMENTIA AND CANNOT LEAVE THE HOUSE
- Keep the routines the usual schedule, activities and breaks from day to day.
- Even if you can't go outside, it's important to keep your body going. Walk inside, stretch gently, move even a few steps.
- Encourage your caregiver to participate in whatever is possible and meaningful for them. It may feel good to get involved in things like clapping on the balcony, bingos or other community actions.
- Take care of medication and food. Don't forget to include something special on the menu from time to time.
- If the person you care for asks questions or shows concern, respond with simple, reassuring and practical messages.
- Try to keep the atmosphere at home quiet. Watch a film on TV or YouTube, listen to entertainment programmes on the radio, communicate with people you know on the tablet... will help you enjoy a good time.
- Music is always a good ally. You can take advantage of it to remember songs that you like or, if possible, to dance. It will serve as a good physical exercise and will help to maintain the mood.
- Taking the air together through the window, or on the balcony is healthy and helps to maintain contact with the outside world.
- Remember that humor and the expression of affection are good allies for a good day-to-day life.
- Take care of yourself. Talk to friends, share with other caregivers, set aside some time for yourself and ask for help if you need it. Your well-being guarantees that of the person you care for.

9 RECOMMENDATIONS IF YOUR FAMILY MEMBER IS IN HOSPITAL ISOLATION
- Remember that this separation is not your fault. Although as a caregiver you want to do everything you can for your family member and it is difficult to accept what you cannot, it is important to accept the limitations of the situation and remind yourself that it is the external circumstances, not your fault, that prevent you from being by their side now.
- Practice being calm. Letting ourselves be carried away by an excess of negative emotions creates added suffering and does not allow us to think clearly. It is normal to feel negative emotions. Accept them. Then practice a relaxation technique, breathing, yoga or mindfulness to help you stay calm. By simply pausing for three deep breaths when you remember, you help regulate emotional distress.
- Trust that your family member is in good hands. Realize that, even though you are not there, your family member has people around, professionals who provide the care he or she needs.
- Trust that your family member is able to adapt to the situation. Human beings have a great capacity to adapt to adverse situations. When a family member is sick, we often think about their vulnerability; but let's not forget that they also have resources and can develop even more inner strength in this new situation.
- Reflect on how you would like to handle this difficult situation. You too are in the process of adapting. Ask yourself the question of how you would like to handle this situation and make it your personal goal to achieve it little by little.
- Communicate with him/her. If you have the possibility to phone or send him/her letters, use these alternative ways of communication. If you can't reach them now, write letters or videotape them, etc., with the intention of being able to give them these at a later date.
- Instead of worrying, connect with positive feelings about your family member. It's normal to have repeated thoughts of worry. Start by accepting them when they appear. To keep it from overwhelming you, connect with positive memories and the feelings of affection and/or gratitude you have for your family member. If you have religious beliefs, or spiritual beliefs in general, you can pray for him or her or use visualization.
- Give yourself permission to rest and replenish your strength. The role of caregiver leads to fatigue and sometimes even exhaustion. However, we take much better care when we have energy and are rested. Take this opportunity to get your strength back now by resting and caring for yourself.
- Learn to accept what you can't control. In general, we like to control as much as we can. However, there are circumstances in life that are beyond our control and are simply as they are. The more we accept life as it is, the less we suffer.

9 RECOMMENDATIONS FOR COMPASSIONATE TELEPHONE COMUNICATION DURING COVID-19
- Get ready to call. with a deep breath and becoming aware of how you want to convey information from compassion.
- Introduce yourself with your name and profession. "I'm... the doctor who's taking care of your father."
- Speak slowly and in short sentences, bearing in mind that emotional disturbance makes it difficult to assimilate information.
- Use simple language, avoiding jargon and technical terms.
- Transmits information in small doses with pauses between them, giving them time to assimilate it.
- It accepts silence, giving space for emotional expression. "Don't worry, there's no rush. I understand this is a very difficult time."
- After the bad news, it conveys some hope or a positive fact. "We're going to take good care of him, make him as comfortable as possible." Or "It's been very quiet until the end."
- Before you finish, invite him to ask questions. "Can you think of anything else you need to know?"
- It offers a continuity of communication or support. "I'll try to call you every day during the admission" or "I'll give you the number of the psychology service in case you want to have a support in these next days."
- After you hang up, take care of yourself, by, for example, discussing with a colleague what it was like.

